Understanding Peripheral Neuropathy: If your feet burn after walking around all day, or your hands feel like they’re tingling when you’re just sitting down watching TV, you’re not alone. You could be showing signs of Peripheral Neuropathy—a condition that affects over 20 million Americans according to the National Institute of Neurological Disorders and Stroke (NINDS). Peripheral neuropathy sounds complicated, but it’s really about one thing: nerve damage. It happens when the nerves outside your brain and spinal cord stop working properly. These are your “peripheral nerves,” and they control how you move, feel, and even how your organs function. This article breaks it all down in plain English. Whether you’re a healthcare worker, someone living with diabetes, or simply curious about why your hands and feet feel funny, this guide will help you understand, manage, and prevent peripheral neuropathy—without the medical jargon.
Table of Contents
Understanding Peripheral Neuropathy
Peripheral neuropathy is common, but it doesn’t have to control your life. Understanding the symptoms and causes helps you act early, while lifestyle changes—like controlling blood sugar, eating well, and staying active—can dramatically improve your quality of life. With new therapies on the horizon and proven methods like exercise and vitamin therapy, there’s real hope for anyone living with nerve pain. The best approach? Stay proactive, informed, and consistent. Your nerves may be delicate, but your ability to heal and adapt is powerful.
| Topic | Key Insights & Stats (2025) |
|---|---|
| Definition | Peripheral neuropathy is nerve damage affecting the nerves outside the brain and spinal cord. |
| Prevalence | Over 20 million Americans live with some form of neuropathy |
| Leading Cause | Diabetes—responsible for nearly 70% of all cases in the U.S. |
| Top Symptoms | Tingling, numbness, burning pain, weakness, loss of coordination. |
| Treatment Options | Blood sugar control, physical therapy, medication, nerve stimulation, vitamin supplements. |
| Emerging Therapies | Regenerative medicine, stem cell therapy, and wearable nerve stimulators are being tested in 2025. |
| Prognosis | Early diagnosis improves outcomes and can reverse mild nerve damage. |
| Official Source | Visit Mayo Clinic’s Peripheral Neuropathy Guide. |
Understanding Peripheral Neuropathy
Peripheral neuropathy happens when the network of nerves that connect your brain and spinal cord to the rest of your body gets damaged or disrupted. These nerves act like electrical wires, carrying signals that control movement, sensation, and organ functions. When they’re damaged, those signals become distorted—or stop entirely.
Imagine your phone charger cable fraying. It might still work sometimes, but the connection is weak and unpredictable. That’s what happens in your body with neuropathy—messages between your brain and your limbs get scrambled.
Peripheral neuropathy can affect:
- Sensory nerves, which control touch and pain.
- Motor nerves, which control movement and muscle strength.
- Autonomic nerves, which control involuntary actions like digestion and heartbeat.
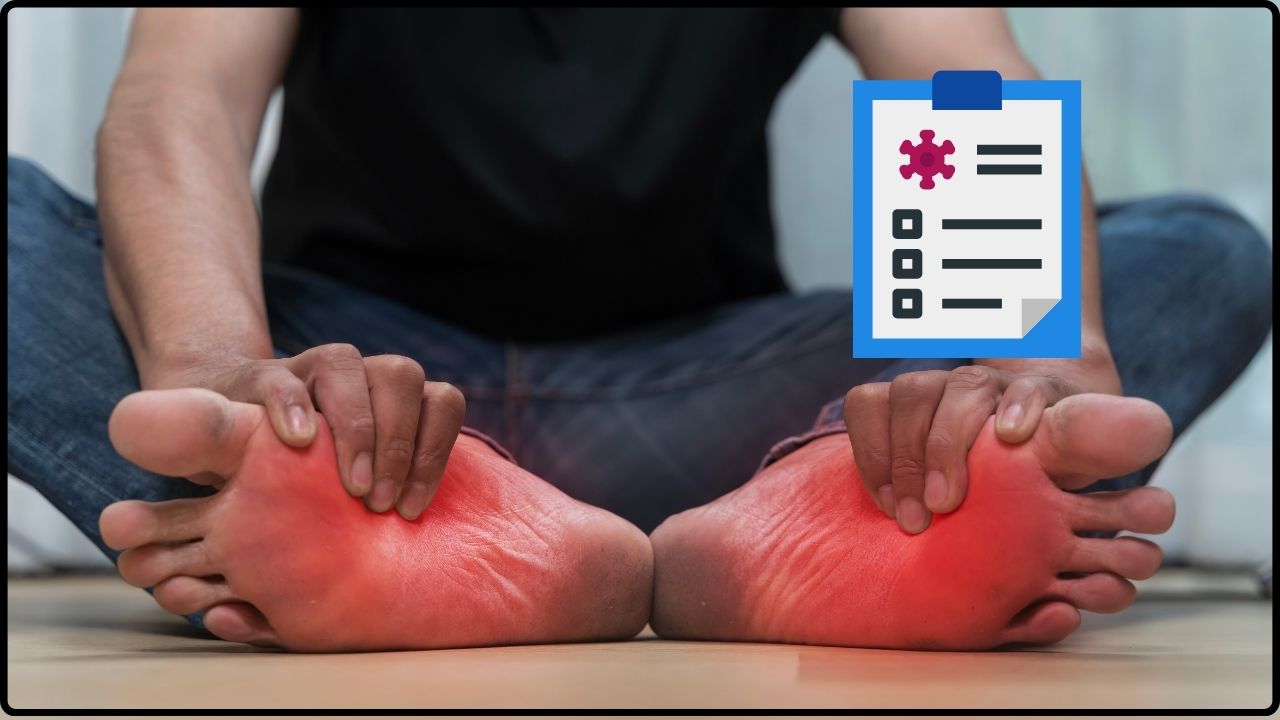
Recognizing the Symptoms of Peripheral Neuropathy
Symptoms vary depending on which nerves are damaged, but they often start in your feet and hands before moving upward. Common signs include:
- Tingling or “pins and needles” feeling in hands or feet
- Burning, stabbing, or electric-shock-like pain
- Numbness that spreads gradually
- Muscle weakness or loss of coordination
- Extreme sensitivity to touch (even light fabric can hurt)
- Balance problems or frequent falls
- Digestive issues, dizziness, or irregular heartbeat (if autonomic nerves are involved)
Many patients describe it as “walking on hot coals” or feeling like they’re wearing socks when they aren’t. These sensations can interfere with daily life, making it hard to sleep, drive, or even button a shirt.
Major Causes of Peripheral Neuropathy
There are many possible triggers. Some cases develop slowly over years, while others appear suddenly after an injury or illness.
1. Diabetes: The Top Culprit
Diabetes is the number one cause of peripheral neuropathy in the United States. According to the Centers for Disease Control and Prevention (CDC), up to 70% of people with diabetes will develop nerve damage during their lifetime.
High blood sugar damages the small blood vessels that supply the nerves, cutting off oxygen and nutrients. This is called diabetic neuropathy, and it often starts in the feet.
2. Vitamin Deficiencies
Your nerves need nutrients—especially vitamin B12, B1 (thiamine), and vitamin E—to stay healthy. People with digestive disorders, alcohol dependency, or restrictive diets (like veganism without supplementation) can develop deficiencies leading to neuropathy.
3. Alcohol Use and Toxins
Heavy drinking over time can cause what’s called alcoholic neuropathy. Alcohol reduces levels of B vitamins and damages nerve tissue directly.
Exposure to industrial toxins like lead, mercury, or arsenic can also cause nerve injury.
4. Autoimmune Diseases
Conditions such as lupus, rheumatoid arthritis, or Guillain-Barré syndrome cause the immune system to mistakenly attack healthy nerves. This can lead to chronic inflammation and nerve fiber destruction.
5. Infections and Injuries
Certain infections like HIV, Lyme disease, shingles, or hepatitis C can damage peripheral nerves.
Physical injuries from accidents, falls, or repetitive stress (like carpal tunnel syndrome) can also compress or sever nerves.
6. Genetic and Idiopathic Neuropathies
Some people inherit genetic nerve disorders like Charcot-Marie-Tooth disease, which cause progressive muscle weakness and sensory loss.
And sometimes, despite extensive testing, doctors can’t find a cause—this is known as idiopathic neuropathy.

How Doctors Diagnose Peripheral Neuropathy?
Diagnosis starts with a detailed medical history and a neurological exam. Your doctor will likely ask when symptoms began, whether you have chronic conditions (like diabetes), and if you’ve been exposed to toxins or heavy alcohol use.
Common diagnostic tests include:
- Nerve conduction studies to measure electrical activity.
- Electromyography (EMG) to check how muscles respond to nerve signals.
- Blood tests for diabetes, vitamin deficiencies, thyroid issues, or autoimmune markers.
- Nerve or skin biopsy in rare cases to study nerve fiber density.
According to the Cleveland Clinic, early detection greatly increases your chances of preventing permanent damage.
Treatment Options: Taking Back Control
While there’s no single cure for all types of neuropathy, treatment focuses on managing the root cause, easing symptoms, and preventing further damage.
1. Treat the Underlying Condition
- For diabetes, keep your A1C below 7% to slow or stop nerve damage.
- For vitamin deficiency, take supplements as prescribed.
- For autoimmune diseases, medications like corticosteroids or immunoglobulin therapy can help.
- If neuropathy is caused by a toxin or drug, removing the source is essential.
2. Manage Pain
Neuropathic pain can be tough to treat with regular painkillers. Doctors may prescribe:
- Prescription drugs like duloxetine (Cymbalta), gabapentin (Neurontin), or pregabalin (Lyrica).
- Topical treatments such as lidocaine patches or capsaicin cream.
- Alternative therapies including acupuncture, biofeedback, and relaxation techniques.
A 2024 study from Harvard Health Publishing found that regular aerobic exercise (even brisk walking) improved nerve sensitivity and reduced pain perception in patients with mild neuropathy.
3. Physical and Occupational Therapy
Therapy can help you regain strength, coordination, and balance.
Occupational therapists can also recommend tools like braces, supportive footwear, or ergonomic changes at work.
4. Emerging Treatments (2025 Update)
Recent research shows promise in:
- Stem cell therapy to regenerate damaged nerve fibers.
- Nerve growth factor (NGF) injections to stimulate repair.
- Wearable nerve stimulators that improve circulation and nerve signaling.
While these are still under clinical trials, they represent hope for millions dealing with chronic nerve pain.
Preventing Peripheral Neuropathy
The best treatment is prevention. Here’s how you can lower your risk:
- Control blood sugar if you’re diabetic or pre-diabetic.
- Eat a balanced diet rich in B vitamins, omega-3 fats, and antioxidants.
- Limit alcohol to no more than one drink per day for women and two for men.
- Exercise for at least 30 minutes five days a week.
- Quit smoking—nicotine restricts blood flow to nerves.
- Protect your feet with comfortable shoes and regular checks for sores or cuts.
For those working physically demanding jobs—nurses, factory workers, truck drivers—wearing supportive footwear and taking short movement breaks can help prevent nerve compression and blood circulation problems.
Living with Peripheral Neuropathy
Living with neuropathy requires patience, but it’s absolutely manageable. Many Americans live full, active lives with the condition. The key is consistency—staying on top of treatment, monitoring your symptoms, and maintaining healthy habits.
Lifestyle tips that help:
- Get plenty of rest and reduce stress.
- Avoid extreme temperatures that can worsen nerve pain.
- Try yoga or tai chi for gentle movement and balance.
- Use assistive devices like canes or braces if needed.
Joining a support group—such as Neuropathy Commons—can also help you connect with others and learn practical coping strategies.

When to See a Doctor?
Seek medical attention if you notice:
- Persistent numbness, tingling, or burning sensations
- Weakness or loss of coordination
- Foot ulcers or infections that don’t heal
- Dizziness, fainting, or digestive irregularities
Ignoring early signs can make recovery harder. The sooner you get evaluated, the more options you have for treatment and recovery.
Essential Endodontic Kits: The Complete Checklist for Setting Up Your Dental Clinic.
Pioglitazone vs. Rosiglitazone: A Review of Thiazolidinediones in Type-2 Diabetes.
Maxillofacial Prosthetics: Techniques for Finger and Facial Rehabilitation